Background
The Affordable Care Act (ACA) gave States the option to expand Medicaid eligibility criteria. Health insurance plays a notable role in health care access and receipt of services, but we know little about coverage rates for low-income cancer survivors and their receipt of cardiovascular-related preventive screenings. This study was conducted to assess the impact of the ACA on cardiovascular preventive screenings for cancer survivors who sought care at community health centers (CHCs).
Useful Findings
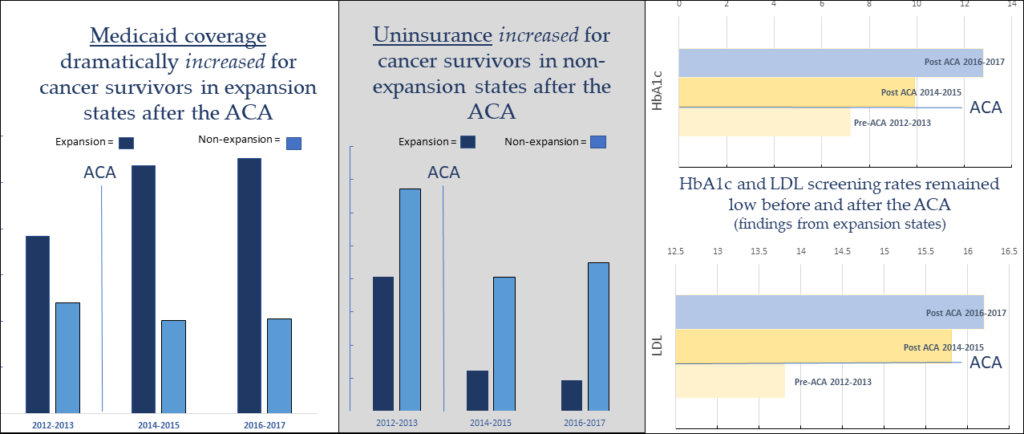
The amount of uninsured cancer survivors in CHCs went down dramatically in Medicaid expansion states, but only modestly in non-expansion states. Meanwhile, Medicaid coverage rates for cancer survivor patients in CHCs surged in expansion states. Blood pressure and body mass index screenings were high for this population before and after the ACA; receipt of low-density lipoproteins and hemoglobin A1c screenings were low and only saw a small increase over time. Despite the difference in health insurance coverage rates between expansion and non-expansion states, there was little increase in cardiovascular-related screenings for cancer survivors in CHCs overall.
Bottom Line
This study, published in the journal Cancer, found a substantial decline in uninsured visits among cancer survivors in Medicaid expansion states. Yet, 1 in 5 cancer survivors living in a state that did not expand Medicaid remained uninsured. Several ACA provisions likely worked together to increase cardiovascular-related preventive screening rates for cancer survivors seen in CHCs.