Background
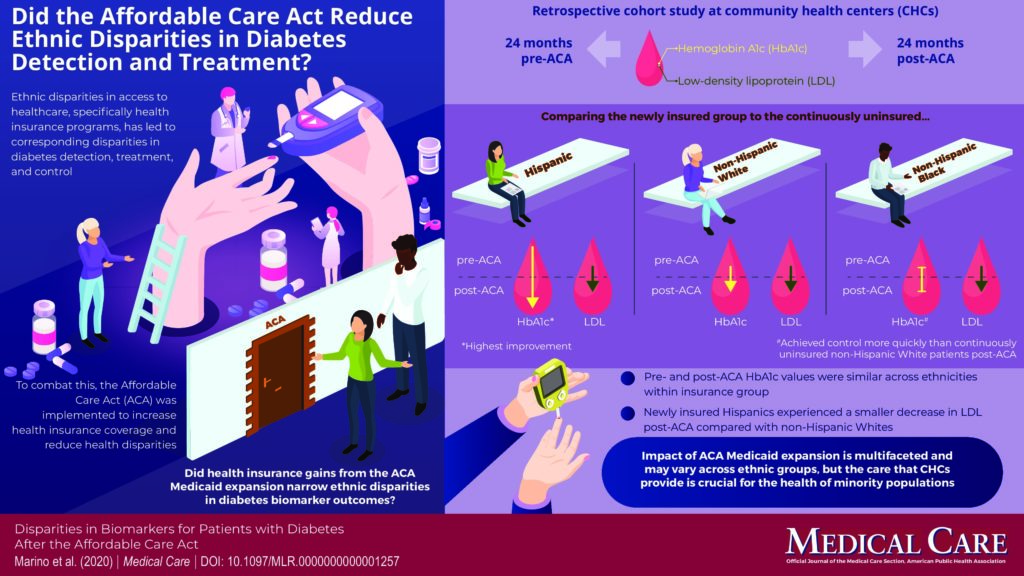
Racial and ethnic minorities are at higher risk for poor diabetes-related outcomes [such as high hemoglobin A1c (HbA1c) and low-density lipoprotein (LDL)] than non-Hispanic whites, yet minorities are less likely to receive diabetes-related services due to multiple factors including insufficient access to health insurance coverage. The Affordable Care Act (ACA) aimed to improve access to health insurance coverage and reduce health disparities. This retrospective, cohort study at community health centers (CHCs), which provide healthcare to underserved populations, evaluated whether gaining health insurance from the ACA Medicaid expansion diminished racial/ethnic disparities in diabetes-related biomarkers for patients with diabetes.
Useful Findings
There was no evidence of significant disparities in diabetes-related biomarkers pre- or post-ACA. However, post-ACA the improvement in mean HbA1c between newly insured and continuously uninsured was significantly greater for Hispanics than non-Hispanic whites. The estimates comparing non-Hispanic black and non-Hispanic whites were not significantly different. Newly insured Hispanics and non-Hispanic whites reduced their LDL more than the continuously uninsured. The results also showed that non-Hispanic whites in all insurance groups had better improvement in LDL from pre-ACA to post-ACA compared with Hispanic and non-Hispanic black patients.
Bottom Line
This study published in Medical Care indicated that the impact of ACA Medicaid expansion is complex and may differ across racial/ethnic groups. Further, the study underscored the benefit of CHCs for the health of minority populations.