Background
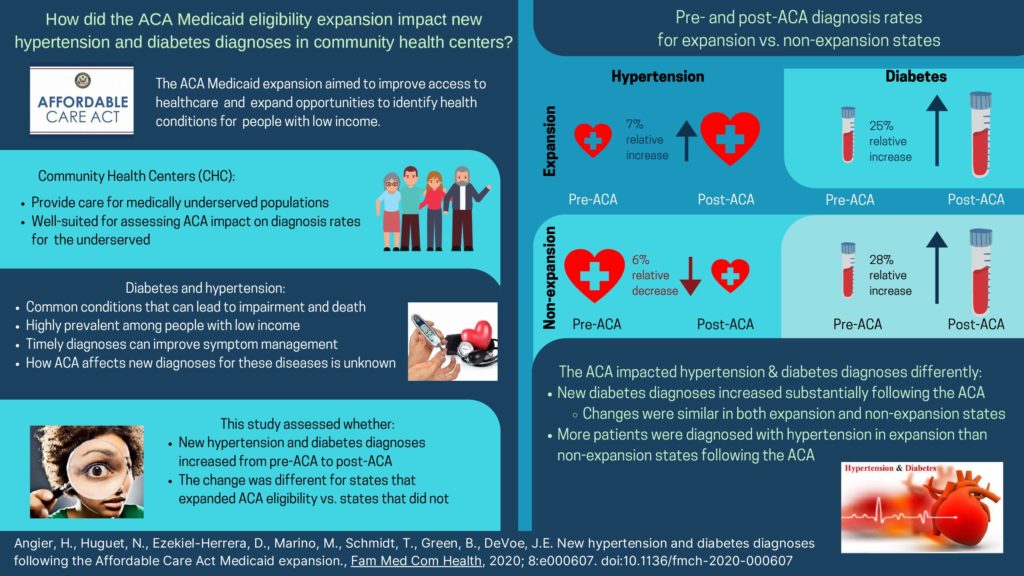
The Affordable Care Act (ACA) Medicaid eligibility expansion aimed to improve access to healthcare and reduce disparities for patients in the US. There is growing evidence that the ACA benefitted patients with low income and led to a decreased number of uninsured and increased preventive health screenings, but little is known about the impact of the ACA on diagnosing medical conditions. Hypertension and diabetes, common health conditions with high risk for disability and death, are on the rise in the US. Timely diagnosis of hypertension and diabetes is the first step to ensure treatment and symptom management. Patients with low income are at higher risk for developing these conditions than those with higher incomes but they may be less likely to receive a timely diagnosis due to barriers accessing healthcare such as lack of insurance or inability to pay for testing. This study evaluated the ACA impact on new hypertension and diabetes diagnoses among a large cohort of patients from community health centers that serve primarily underserved populations.
Useful Findings
Hypertension diagnosis rates differed by expansion status: there was a 6% relative increase in expansion states and a 7% relative decrease in non-expansion states post-ACA. Rates of new diabetes diagnoses increased substantially pre-ACA to post-ACA in both expansion (25% relative increase) and non-expansion (28% relative increase) states.
Bottom Line
This study published in Family Medicine and Community Health showed differential impact of the ACA Medicaid expansion on hypertension and diabetes diagnosis rates. Following the ACA expansion, diagnosis rates for diabetes increased substantially regardless of expansion status, while more patients were diagnosed with hypertension in expansion compared to non-expansion states following the ACA. These findings suggest that increased ACA-related health insurance opportunities may have facilitated access to diagnostic tests to detect diabetes for patients served by community health centers.